Case #1: The Recall That Vanished And the Lawsuit That Followed
The System Failed. And Mr. Skinner Paid the Price.
A 53-year-old man, tired all the time, walks into his GP surgery. Dr. Lee runs bloods. The result: Hb 10.7 (anaemia). A red flag. Dr. Lee issues a simple instruction: "Recall him for a follow-up."
But the message disappears into the void.
The patient: Unreachable. The recall: Lost in the black hole of ad-hoc processes.
One year later, Mr. Skinner is back. But this time, it’s too late. He’s rushed through the two-week wait pathway. The diagnosis: Metastatic colorectal cancer. The outcome: A lawsuit.
Dr. Lee and every other GP involved is dragged into the legal crosshairs.
BookYourGP: Because ‘Lost in the System’ is Not an Option
With BookYourGP, recalls don’t vanish. They are locked, tracked, and actioned with military-grade precision.
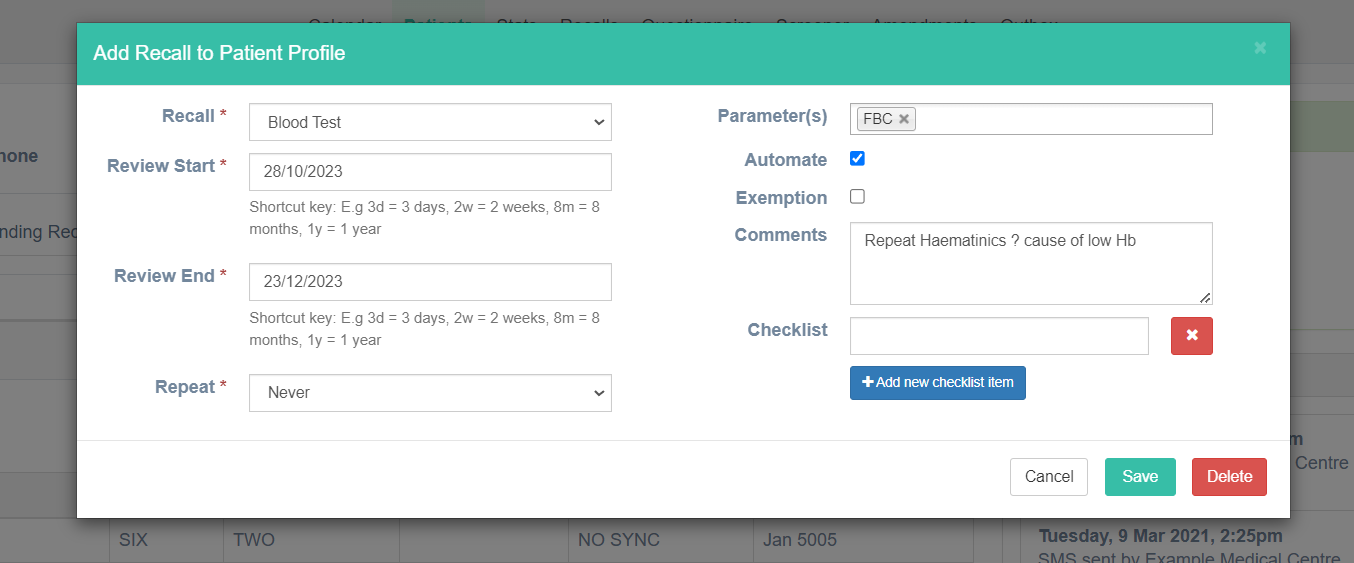
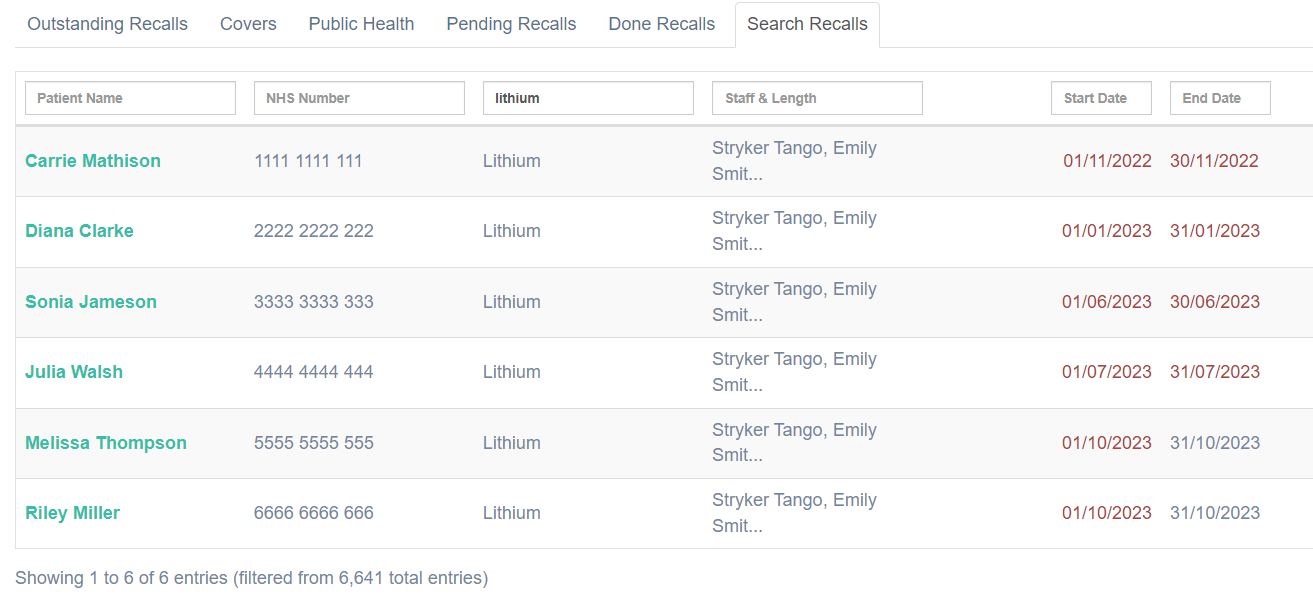
- Save Recalls with One Click – Every recall is tied to the patient’s record. No more ‘lost messages’.
- Automated Follow-Ups – The patient gets reminders until action is taken. No more ‘we couldn’t reach them’.
- Read-Coded & Medico-Legally Secure – Every step is recorded and auditable. No more ‘but we told the team to follow up’.
This is how you protect your patients and yourself.